Case of the month
Dr. Vaibhav Nasre

This is a rare case report of 20 year old female presented with headache and raised icp features due to hydrocephalus. Vp shunt was done for hydrocephalus and tumour resection has been explained to family . She is under follow up . Neurological deficits is one of the indication for tumour resection .
Dysplastic cerebellar gangliocytoma, perhaps better known as Lhermitte-Duclos disease, is a rare tumor of the cerebellum appearing as thickening and increase in T2 signal of the cerebellar folia giving this lesion a characteristic striated appearance.
Dysplastic cerebellar gangliocytomas typically present in young adults, although they have been encountered at all ages.
Small tumors may be asymptomatic or only present with relatively subtle cerebellar signs (e.g. dysmetria). When larger, symptoms are typically related to raised intracranial pressure, obstructive hydrocephalus and to a lesser degree, cerebellar dysfunction.
The dysplastic mass grows very slowly, and initial treatment revolves around treating hydrocephalus. Surgical resection is often curative, with only a few case reports of recurrence 3. Importantly it is crucial to remember the association with Cowden syndrome, hence, increased risk of other neoplasms such as breast, endometrial and thyroid cancers. Therefore, a recommendation for further imaging or clinical assessment of possible tumors in these locations should be included in the radiologist’s report.
Brush Sign in Cortical Venous Sinus Thrombosis
Dr. Mandar Waghralkar
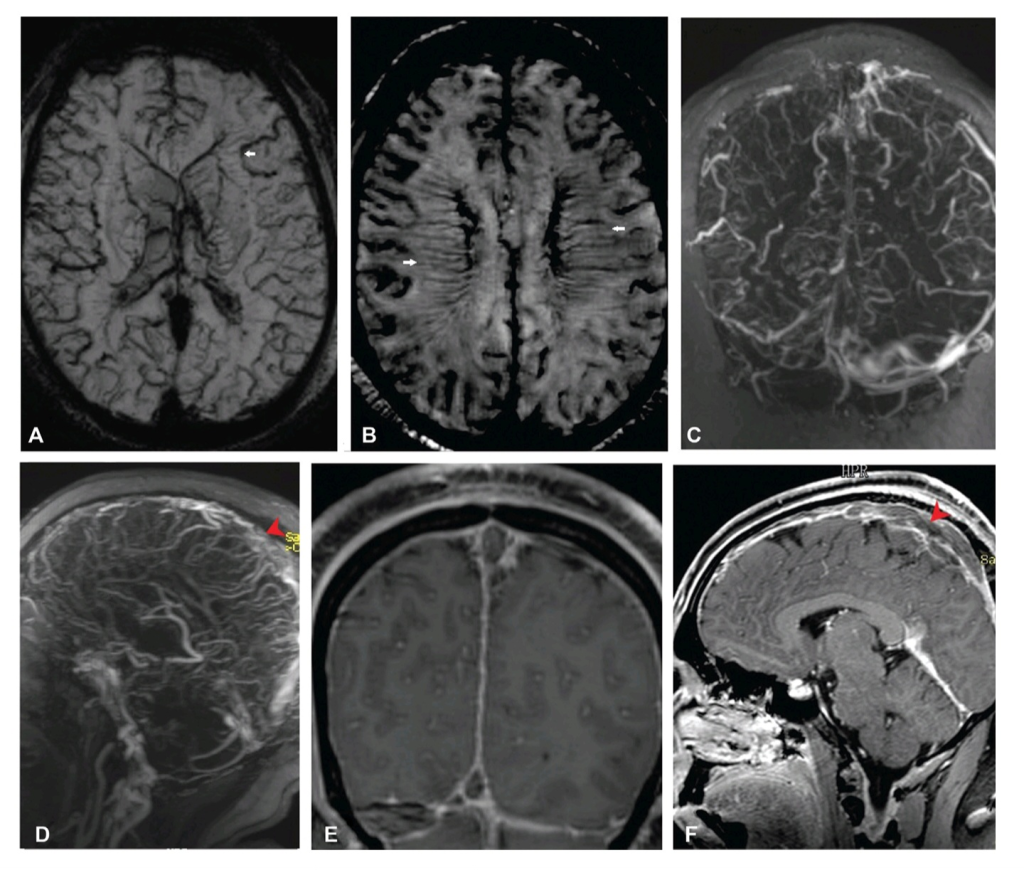
Brushsign(BS) is a MRI sign seen in CVST suggestive of dilatation with blooming artifacts involving the superficial cortical veins of both the cerebral hemispheres due to congestion. Paramagnetic sensitive MR sequences (SWI and T2-weighted imaging [T2WI]) allow better visualization of these veins, particularly in the conditions associated with high intravenous deoxyhemoglobin.
The BS manifests as an abnormal decrease in signal intensity of the subependymal and deep medullary veins on paramagnetic-sensitive MRI sequences seen in few patients of cerebral venous sinus thrombosis (CVST) and that too with a high thrombus load. An alternative explanation of the BS is the development of collateral venous pathways between the superficial and deep venous systems of the brain, seen on postcontrast images. Additionally, the BS has also been described in other pathological conditions, such as the moyamoya disease or Sturge–Weber syndrome.
Axial gradient echo sequence(GRE)images show dilatation with blooming artifacts seen in the superficial cortical veins of both the cerebral hemispheres due to congestion(small white arrows),the brush sign.(C,D) Contrast magnetic resonance venography(MRV) coronal and sagittal images and (E, F) postgadolinium sagittal and coronal T1-weighted images show replacement of normal flow-related signal void and absence of contrast opacification of these segment of the dural venous sinuses suggestive of thrombosis involving superior sagittal sinus (red pointed arrowheads), torcular herophili, and right-sided transverse sigmoid sinus, proximal third of the left transverse sinus and straight sinus, and vein of Galen, also extending to the right internal jugular vein.
The BS manifests as an abnormal decrease in signal intensity of the subependymal and deep medullary veins on paramagnetic-sensitive MRI sequences seen in few patients of cerebral venous sinus thrombosis (CVST) and that too with a high thrombus load. An alternative explanation of the BS is the development of collateral venous pathways between the superficial and deep venous systems of the brain, seen on postcontrast images. Additionally, the BS has also been described in other pathological conditions, such as the moyamoya disease or Sturge–Weber syndrome.
Axial gradient echo sequence(GRE)images show dilatation with blooming artifacts seen in the superficial cortical veins of both the cerebral hemispheres due to congestion(small white arrows),the brush sign.(C,D) Contrast magnetic resonance venography(MRV) coronal and sagittal images and (E, F) postgadolinium sagittal and coronal T1-weighted images show replacement of normal flow-related signal void and absence of contrast opacification of these segment of the dural venous sinuses suggestive of thrombosis involving superior sagittal sinus (red pointed arrowheads), torcular herophili, and right-sided transverse sigmoid sinus, proximal third of the left transverse sinus and straight sinus, and vein of Galen, also extending to the right internal jugular vein.
An Extremely Rare Anomalous Variation of left Anterior cerebral artery (ACA)in a Patient with SDH
Dr. Mandar Waghralkar
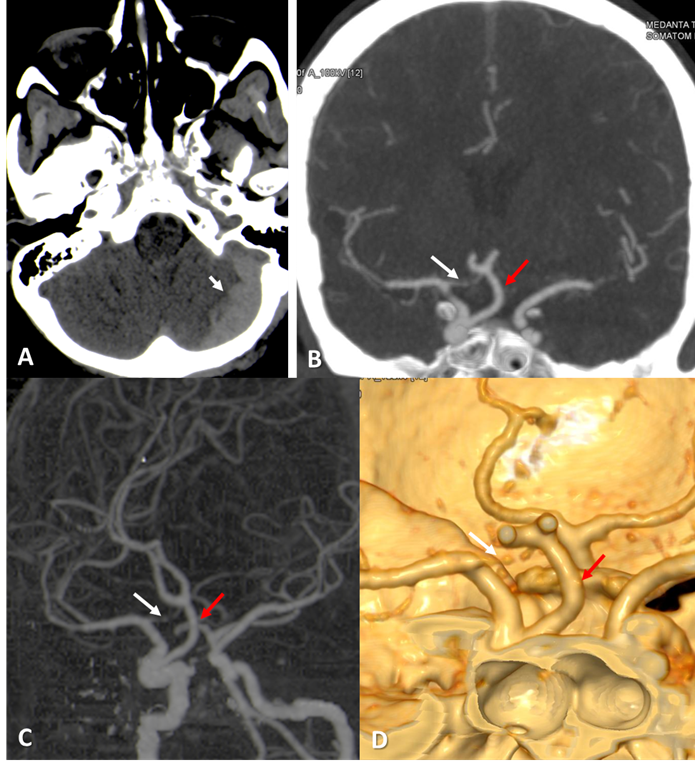
The anterior cerebral artery (ACA) usually arises from the Internal carotid artery(ICA) terminus and extends anteromedially to join the Anterior communicating artery (ACoA). There are many anomalies of A1 segment ACA described in the literature by several authors. The anomalies include hypoplastic or aplastic arteries, fenestration of ACA, accessory or duplicated ACA and persistent primitive olfactory artery However, ICA origin of contralateral ACA is extremely rare anomaly. Only three cases of anomalous origin of contralateral ACA from ICA has been reported in the literature.It is unique from the three previously reported cases in having left ACA origin from the contralateral paraclinoid ICA with hypoplastic A1 segment of right ACA.
These ACA anomalies are incidentally detected in angiography however their association with other coexistent anomalies including aneurysm, AVM, Moya-Moya disease and compressive symptoms of optic apparatus have been well documented in literature.
It is an extremely rare anomalous variation of left anterior cerebral artery arising from the contralateral paraclinoid Internal carotid artery with hypoplastic right ACA. Angiographic identification and characterisation of this anomaly is very important in developing a differential diagnosis and when planning a surgery and endovascular procedure.
A Computed tomography of head shows acute subdural hemorrhage (white short arrow) along the left cerebellar hemisphere. B,C,D Coronal maximum-intensity-projection (MIP) image and 3 Dimensional Volume rendering images of CT angiography shows origin of left anterior cerebral artery from the right paraclinoid Internal carotid artery (Red arrow) and right anterior cerebral artery is hypoplastic (white arrow) arising from the right Internal carotid artery terminus.
These ACA anomalies are incidentally detected in angiography however their association with other coexistent anomalies including aneurysm, AVM, Moya-Moya disease and compressive symptoms of optic apparatus have been well documented in literature.
It is an extremely rare anomalous variation of left anterior cerebral artery arising from the contralateral paraclinoid Internal carotid artery with hypoplastic right ACA. Angiographic identification and characterisation of this anomaly is very important in developing a differential diagnosis and when planning a surgery and endovascular procedure.
A Computed tomography of head shows acute subdural hemorrhage (white short arrow) along the left cerebellar hemisphere. B,C,D Coronal maximum-intensity-projection (MIP) image and 3 Dimensional Volume rendering images of CT angiography shows origin of left anterior cerebral artery from the right paraclinoid Internal carotid artery (Red arrow) and right anterior cerebral artery is hypoplastic (white arrow) arising from the right Internal carotid artery terminus.
